BRCA 1 mutations role in PCa questioned, Oh, God!, prostate cancer myths, team approach needed for BPH, a drug recall
By Howard Wolinsky
Here are the latest nuggets on prostate health extracted from the medical literature and more:
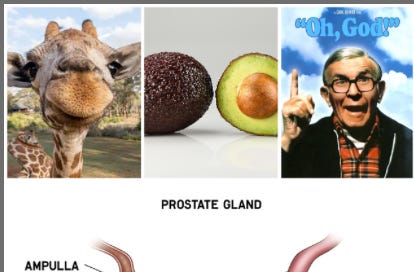
—God (played by George Burns in the 1977 movie “Oh, God!”) was asked about the mistakes He had made. He listed tobacco and giraffes. And avocados. “Did you see the pit?” And also He allegedly listed the prostate. With all the fuss with BPH, cancer and prostatitis. Note the finger in the move poster. Would DREs make the list?
—I was clear that BRCA 2 mutations were linked not only to Breast Cancer, its original target), but prostate and a few other cancers. But the message on the BRCA 1 mutation and a link to prostate cancer seemed fuzzy.
A new study appearing in BMJ Oncology suggests that BRCA 1 may not initiate prostate cancer and that it may be time to time to reassess current treatment with PARP (poly(ADP-ribose) polymerase) inhibitor drugs, which block the ability of cells, including cancer cells, to repair DNA damage, in men with BRCA1 genetic variants.
Dr. D. Gareth Evans, of Manchester Academic Health Science Centre, Manchester, UK, and colleagues said: Germline BRCA2 pathogenic variants (PVs) are known to cause ~4% of prostate cancer, but other homologous repair genes, BRCA1, ATM, PALB2 and Lynch syndrome genes are also involved. Our objective was to assess the contribution of germline [inherited] and somatic [acquired] gene variants to prostate cancer.”
Researchers said: “BRCA2 is the most frequently identified prostate cancer gene with over 10% involvement in metastatic disease. BRCA2 and CDK12 somatic PVs do not appear to be mutually exclusive. BRCA1 does not appear to be a significant contributor to prostate cancer progression.”
In an editorial, Fumihiko Urabe, MD, PhD, of the Jikei University School of Medicine in Minato, Japan, and Kosuke Takemura, MD, PhD, of the Cancer Institute Hospital of the Japanese Foundation for Cancer Research in Tokyo, said the new study could help refine genetic testing and personalized treatment of patients with PCa. They said it may be time to reevaluate current treatment guidelines, noting that the new data "reinforce the role of BRCA2 and ATM as key determinants of aggressive prostate cancer phenotypes."
—Calling all Chicagoans on Active Surveillance for low-risk prostate cancer. I have had a flurry of emails from you after NOT hearing from you for years, My The ActiveSurveillor.com newsletter is organizing a lunch at 11:30 a.m. Central March 20. Contact me at howard.wolinsky@gmail.com, and I’ll share the deets.
—Here’s a stunning statistic: Approximately 87% of men undergoing prostatectomy report erectile dysfunction (ED) at two years post-op with nerve-sparing techniques offering some improvement, Dr. Mark Perloe, himself a prostate cancer patient and a moderator of the low- to intermediate-risk group at AnCan reports in a newsletter article about the various myths about PCa. Check it out at https://mail.google.com/mail/u/0/#search/AnCan+Mark+Perloe/FMfcgzQZSZJxdSMXJMPvPZqwvSQmZsNr
Other prostate myths? There are loads. PCa is only an old man’s disease. Urinary symptoms indicate prostate cancer: Untrue in lower-grade disease.
—A team approach needed for best results with BPH. Wayne Kuang, MD, an adult urologist from Albuquerque, N.M, thinks it takes a village of health professionals to take on benign prostatic hyperplasia (BPH).
He said in Urology Times that neurologists, endocrinologists, primary care doctors, pharma and the medical device industry, beed to collaborate and take into consideration not only the bladder but the prostate. I’d include gerontologists, nurse practitioners, pelvic floor physical therapists and other health professionals, too. Kuang, who runs a campaign called Man v. Prostate, which “prioritizes Bladder Health while making the best decision for Prostate Care.”
He notes that contributing factors include “aging. As men get older, bladder muscles are also going to get older and get weaker. We need to factor that in. We need to factor in diabetes. How does the effect on diabetic cystopathy, pathologies on the bladder due to diabetes, influence lower urinary tract symptoms or neurologic dysfunctions like multiple sclerosis or Parkinson's disease, or the fact that we now, currently in America, have an epidemic of obesity.”
Was a urinary pun intended, when Kuang noted: "If we synergize our efforts and our energy, as the level of the sea rises, all ships on the sea will rise with it.”
—Recall of BPH drug. The U.S. Food and Drug Administration (FDA) on Jan. 16 he announced a voluntary recall for 7,820 bottles of the precription drug Cardura XL, also known as doxazosin (extended release). The alpha blocker often prescribed to help with urination difficulties associated with enlarged prostate (benign prostatic hyperplasia) symptoms. (The non-extended release version of Cardura is also at times prescribed to treat high blood pressure.)
Cardura XL recall appears to involve issues that arose during stability tests, resulting in “failed impurities/degradation specifications” and “out of specification results.”The FDA categorized it as a Class II recall: “A situation in which use of, or exposure to, a violative product may cause temporary or medically reversible adverse health consequences or where the probability of serious adverse health consequences is remote.”
Consumers can confirm whether their prescriptions are affected by checking for the following details:
Cardura XL (doxazosin) extended release tablets, 8 mg
30-count bottles
Lot # 8181625
Expiration date: 12/31/2025
Cardura XL (doxazosin) extended release tablets, 4 mg
30-count bottles
Lot # 8182298
Expiration date: 10/31/2025
Viatris Speciality LLC, of Morgantown, West Virginia, is the distributor.
—PSA levels and depression? Dr. Yong Huang, of the Department of Urology, The First Affiliated Hospital of Chongqing Medical University, Chongqing, China, report on a link between depression and PSA levels in U.S. men without prostate cancer. “Depression score is inversely correlated with serum total PSA concentrations among American men, and there is an interaction between depression and myocardial infarction,” they said in BMC Psychiatry. “It was important to note that although individuals with moderate and mild depression had significantly lower PSA values compared to those without depression, the actual differences in PSA values may not be clinically significant,” they said.
They suggest these findings could lead to a strategy of improved screening for prostate cancer, reducing issues such as false positives, over-diagnosis, and overtreatment. “Although it is unclear how depression causes a decrease in serum PSA concentrations, one possible reason is that depression affects sex hormone levels in men, especially manifested by a slight increase in estradiol and a significant decrease in testosterone,” they said.
—Resume Rezūm. Lasers, electrical currents, now water vapor. Oh, my.
Our prostates cause so much trouble.
But help may be on the way to “vaporize” enlarged prostates.
A new report describes the use of The Rezūm System (Rezūm: Boston Scientific, Marlborough, MA, USA), which uses water vapor therapy to reduce prostate size.
(I first reported on this “cup of tea” approach to reducing prostate size with barely boiling water. Check this out: https://www.medscape.com/viewarticle/969052)
Mustufa Babar, MD, of Albert Einstein College of Medicine, New York, and colleagues aimed to ID predictors for achieving a minimal clinically important difference (MCID) in LUTS (lower urinary tract symptoms) following Rezūm.
In this study of 174 patients treated with water vapor, there was improvement of equal to or more than 25% in the International Prostate Symptom Score (IPSS). “We found that 77% of patients experienced a clinically significant improvement in LUTS within 3 months of treatment,” they wrote.
Two main predictors of achieving MCID were identified: higher baseline LUTS severity (measured by IPSS) and larger prostate volumes. Patients with severe LUTS and prostate volumes greater than 60 cc were more likely to experience meaningful improvements in urinary function. Notably, our study also shows that symptom improvement is rapid and durable, with patients continuing to see benefits up to 12 months post-treatment.
Further investigation is needed to assess long-term outcomes and retreatment rates, researchers said.
Some research is underway on using the cuppa method for prostate cancer.
The paper was presented at the American Society of Clinical Oncology Genitourinary Cancers Symposium meeting in February in San Francisco.


The authors of this study say, "We show that germline or somatic BRCA1 variants are not a major contributor to prostate cancer." However, this study has significant limitations and is inconsistent with other studies, making its conclusion questionable.
1. The study does not clearly differentiate between biallelic versus monoallelic loss of BRCA1.
2. The study was not a systematic screening of all men presenting with prostate cancer at diagnosis (e.g., aggressive localized or metastatic disease), so the case indices for de novo hormone-sensitive metastatic or localized prostate cancer cannot be calculated with confidence.
3. Because the population tested is relatively newly diagnosed with most diagnostic testing (>80%) in the last 2 years, implications on outcomes and metastatic disease cannot be confidently asserted for BRCA1.
4. The much smaller prevalence of BRCA1 (0.44%) versus BRCA2 (6%) in this study likely limits the statistical power to detect a significant association between BRCA1 mutations and prostate cancer progression
The low frequency of BRCA1 mutations in multiple studies, including this one, makes it challenging to draw firm conclusions about its independent effect on prostate cancer progression.
It is documented that biallelic inactivation of BRCA1 leads to a complete loss of function in homologous recombination repair, resulting in higher genomic instability, which suggests a more aggressive cancer phenotype. Some researchers think that biallelic loss of BRCA1 may be associated with more aggressive prostate cancer because it results in the complete loss of HHR. Definitive studies need to be done to confirm this assertion, as well as the conclusion made in this study.